Attention: Restrictions on use of AUA, AUAER, and UCF content in third party applications, including artificial intelligence technologies, such as large language models and generative AI.
You are prohibited from using or uploading content you accessed through this website into external applications, bots, software, or websites, including those using artificial intelligence technologies and infrastructure, including deep learning, machine learning and large language models and generative AI.
Gonadoblastoma
- Combination of GCT and SCT.
- Mixture of seminoma-like germ cells and immature SCT elements that resemble Sertoli cell tumor or granulosa cell tumor.
- Extremely rare, usually encountered in patients with dysgenetic gonad.
- Most patients are phenotypically female (80%); majority has Y chromosome.
- During embryonic development, immature bi-potential gonads fail to differentiate along male pathway.
- 30% has bilateral testicular involvement.
- Gross: solid yellow-tan nodules with gritty calcifications.
- Histology:
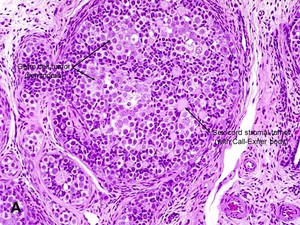
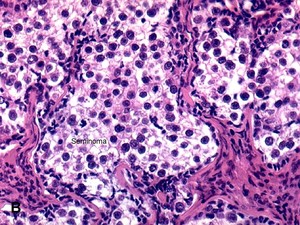
- Well-rounded nests of large pale seminoma-like cells with abundant clear cytoplasm and well-defined cytoplasmic membranes (image A) & (image B).
- Admixed are dark angular sex-cord cells that tend to palisade at the periphery of the tumor nests (looks like Call-Exner bodies).
- Basement membranes can become very hyalinized and even calcified.
- Less often, nodular aggregates of Leydig cells are seen as well.
- Immunohistochemistry: Germ cells: PLAP+, CD117+, Oct3/4+ and stromal cells: inhibin+ or calretinin+.
- Represent pre-malignant lesions from which malignant GCTs can arise; therefore, since majority of patients have gonadal dysgenesis and therefore run a high risk of bilateral tumors, the recommended treatment is bilateral orchiectomy.
advertisement
advertisement